Express News Service
CHENNAI : Despite many advances in medical management and evidence-based dietary interventions, cardiovascular diseases (CVD) still tend to be one of the leading causes of death currently.
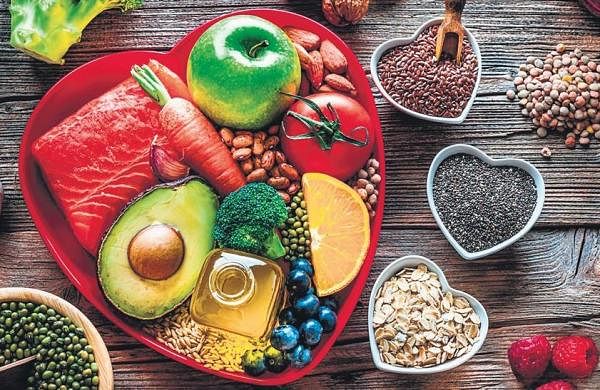
It is important to understand the lifestyle interventions and the different changes one can adapt to reduce the risk of CVD and other illnesses. Lifestyle changes, including a heart-healthy diet, are the foundation of CVD prevention guidelines. The main cardiometabolic risk factors are diabetes, hypertension, dyslipidemia, and excess abdominal fat, which are all affected by dietary changes.
Factors which affect heart health include favourable levels of physical activity, sleep, nicotine exposure, BMI, blood lipids, blood glucose, and blood pressure. Diets rich in fruits, vegetables, legumes, whole grains, and lean protein sources, with minimisation/avoidance of processed foods, trans-fats, and sugar-sweetened beverages, are recommended. The Mediterranean, the Dietary Approaches to Stop Hypertension (DASH), and plant-based diets all have proven cardioprotective in varying degrees and are endorsed by professional healthcare societies. Diets like the ketogenic diet and intermittent fasting still need more research to be proven as cardioprotective.
Dietary patterns
Three dietary patterns ŌĆö The Mediterranean diet, the DASH diet and the plant-based diet ŌĆö have been most studied and proven as cardioprotective.
Mediterranean diet: Rich in poly and mono-unsaturated fats that reduce inflammation and are effective in secondary prevention. The diet is rich in whole grains, leafy green vegetables, fruits, legumes, unsalted nuts, herbs, spices, and extra virgin olive oil (EVOO), with a moderate intake of lean proteins such as fish and poultry, moderate alcohol consumption, and limited intake of red meat and sweets.
By its very nature, the Mediterranean diet limits or eliminates many of the culprits that drive CVD ŌĆö saturated fat, highly processed refined grains and sugars, and red meat. It differs from other dietary patterns as there is a greater emphasis on EVOO, nuts, reduced dairy consumption, and eating with family. This diet has been found to be favourable as a food pattern, rather than single nutrient supplementation, as it inherently provides antioxidants, reduces inflammation of the vascular wall, modulates pro-atherogenic genes, alters the gut microbiome, and improves lipid panels by decreasing low-density lipoprotein cholesterol (bad cholesterol) and raising high-density lipoprotein cholesterol (good cholesterol)
DASH diet: Dietary Approaches to Stop Hypertension emphasises on low salt to help reduce blood pressure. The DASH diet is rich in fruits and vegetables, low-fat dairy, whole grains, poultry, fish, nuts, and seeds while limiting fatty meats, sweets, sugar-sweetened beverages, and full-fat dairy products. The standard DASH diet restricts salt consumption to 2,300 mg per day. A reduced-sodium version of DASH limits sodium intake to 1,500 mg per day. DASH diet shows significant reduction in cardiometabolic risk by lowering blood pressure, total cholesterol and LDL Cholesterol.
Plant-based diet: This diet avoids animal-based products which reduces atherosclerosis (accumulation of fat in the arteries) and improves microbiome diversity (better gut health). The subsets branch into vegetarian (which excludes meat, poultry, seafood, and fish) and vegan (in which all animal food and their products are eliminated from the diet). Other subsets include Lacto-vegetarians, who consume dairy products, lacto-ovo-vegetarians, who consume dairy and eggs, pesco-vegetarians or pescatarians, who consume fish, dairy, and eggs, and semi-vegetarians, who exclude red meats, possibly poultry as well.
The main foundation of a healthy plant-based diet is whole grains, fruits, vegetables, nuts, and legumes with the low frequency and content of animal food. It has low energy density, with low saturated fats and high fibre content, which triggers early satiety cues and helps with digestion by delaying gastric emptying, with moderate insulinemic and glycemic responses along with lowering LDL cholesterol.